On this page:
The Annual Report to the Nation on the Status of Cancer published statistics on new cancer cases, deaths, and trends in the United States. The report includes long-term trends since 2001 and short-term trends with the most recent five years of data, which covers 2017 – 2021 for incidence and 2018 – 2022 for mortality. The Annual Report also provides rates and trends for the most common cancers among children (aged 0 – 14) and adolescents and young adults or AYAs (aged 15 – 39).
The report includes long-term trends since 2001 and short-term trends with the most recent five years of data, which covers 2017 – 2021 for incidence and 2018 – 2022 for mortality. The Annual Report also provides rates and trends for the most common cancers among children (aged 0 – 14) and adolescents and young adults or AYAs (aged 15 – 39).
Scroll down to learn more about trends in cancer incidence and mortality rates.
Cancer Death Rates
Falling cancer death rates are the gold standard when measuring our progress against cancer.
Adults
Overall, from 2018 to 2022, cancer death rates decreased an average of 1.7% per year for men and an average of 1.3% per year for women.
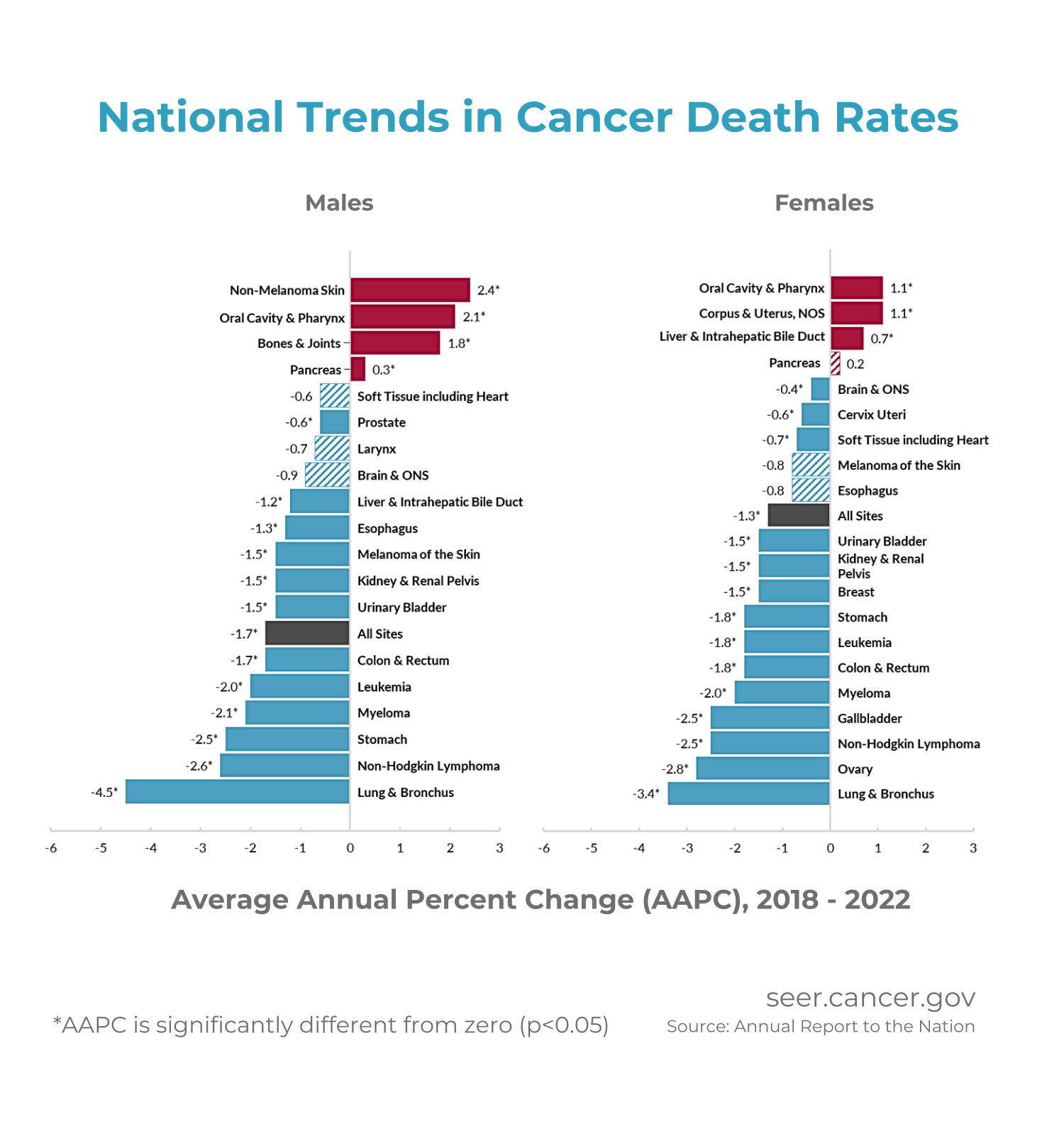
Between 2018 - 2022, 12 of the 19 most common cancers in men showed decreases in mortality :
:
- prostate, liver and intrahepatic bile duct, esophagus, melanoma of the skin, kidney and renal pelvis, urinary bladder, colon and rectum, leukemia, myeloma, stomach, non-Hodgkin lymphoma, and lung and bronchus.
Out of these 12, the death rate from lung and bronchus cancer fell the fastest, dropping by an average of 4.5% each year from 2018 – 2022.
Death rates increased for cancers of the pancreas, bones and joints, oral cavity and pharynx, and non-melanoma skin cancer during this period.
Between 2018 - 2022, 14 of the 20 most common cancers in women showed decreases in mortality :
:
- brain and other nervous system, cervix, soft tissue including heart, urinary bladder, kidney and renal pelvis, breast, stomach, leukemia, colon and rectum, myeloma, gallbladder, non-Hodgkin lymphoma, ovary, and lung and bronchus.
Like the trends seen among men, the death rate from lung and bronchus cancer among women fell the fastest, with an average annual decrease of 3.4% from 2018 – 2022.
Death rates increased for cancers of the oral cavity and pharynx, corpus and uterus, and liver and intrahepatic bile duct for women during this period.
Children and Adolescents and Young Adults (AYAs)
Cancer death rates decreased an average of 1.5% per year from 2001 – 2022 among children. Among AYAs, cancer death rates fell by 2.9% per year from 2001 – 2005, 1% per year from 2005 – 2020, and then remained stable from 2020 – 2022.
Rates of New Cancers
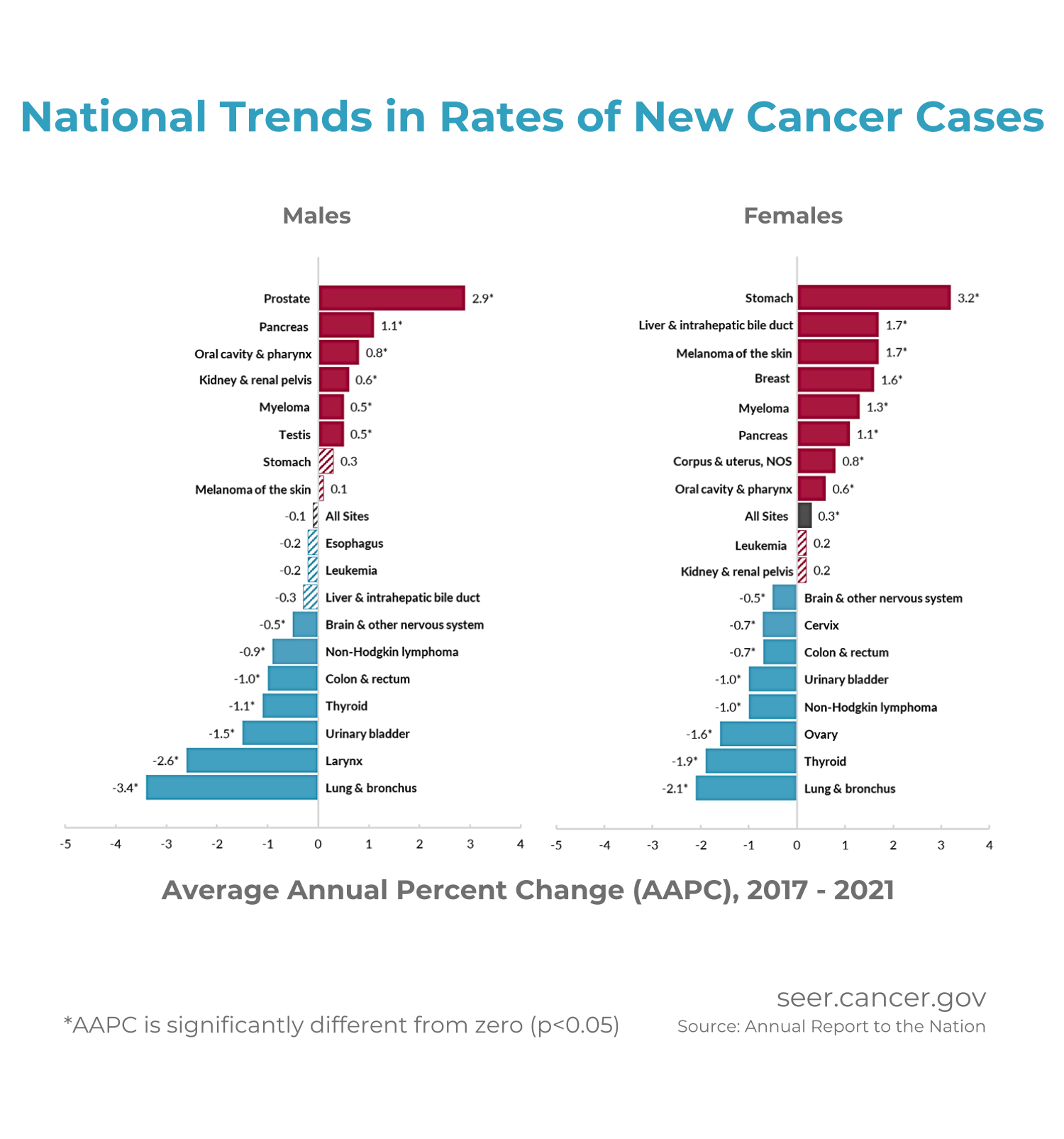
Rates of new cancer cases among men decreased by 1.6% – 2.2% per year from 2001 through 2013 before stabilizing through 2021. Among women, the rate of new cancers increased by 0.3% per year from 2003 through 2021.
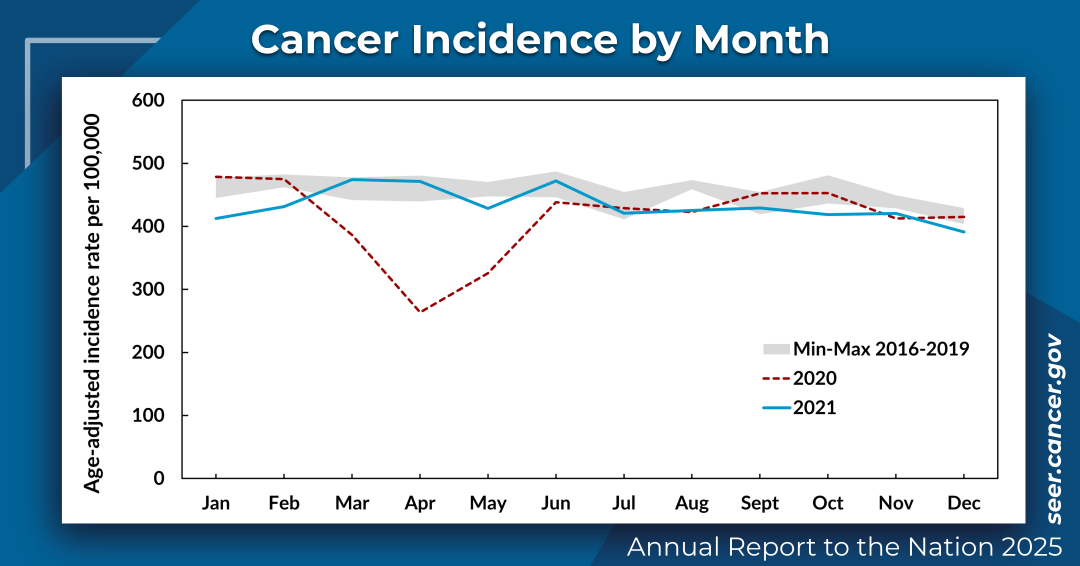
Due to the start of the COVID-19 pandemic in 2020, rates of new cancer cases were 8% lower than expected. The rate of new cases returned to expected levels in 2021. To better understand the underlying cancer burden in the U.S., the report examined cancer case data from 2020 separately and also excluded it from cancer trend analysis.
Among men, incidence rates decreased for 7 cancers between 2017 – 2021:
- brain and other nervous system, non-Hodgkin lymphoma, colon and rectum, thyroid, urinary bladder, larynx, and lung and bronchus.
Rates of new cases did not change much for 5 cancers:
- stomach, melanoma of the skin, esophagus, leukemia, and liver and intrahepatic bile duct.
Meanwhile, incidence rates for 6 cancers increased:
- prostate, pancreas, oral cavity and pharynx, kidney and renal pelvis, myeloma, and testis.
Rates of new lung and bronchus cancers fell the fastest at 3.4% on average per year, while rates of prostate cancer increased the fastest at an average of 2.9% per year.
Among women, incidence rates decreased for 8 cancers between 2017 – 2021:
- brain and other nervous system, cervix, colon and rectum, urinary bladder, non-Hodgkin lymphoma, ovary, thyroid, and lung and bronchus.
Rates of new cases did not change much for:
- kidney and renal pelvis cancer and leukemia.
Meanwhile, incidence rates increased for 8 cancers:
- stomach, liver and intrahepatic bile duct, melanoma of the skin, breast, myeloma, pancreas, corpus and uterus, and oral cavity and pharynx.
Like the rate of new cancer cases among men, rates of new lung and bronchus cancer cases among women fell the fastest at an average of 2.1% per year, while the rate of new stomach cancer cases increased the fastest at an average of 3.2% per year.
Among children, the rate of new cases averaged across all sites and across all racial and ethnic groups fell by 0.8% per year from 2017 to 2021.
The most common cancer types among children included leukemia, brain and other nervous system, and lymphoma. Between 2017 and 2021, the rate of new cases of leukemia and lymphoma increased by an average of 0.5% and 0.6% per year. The rate of new brain and other nervous system cancers among children fell by an average of 2.9% per year during this time.
Among AYAs (aged 15 – 39 years), overall rates of new cancer cases did not change between 2017 and 2021. The most common cancer among AYAs was female breast cancer, followed by cancers of the thyroid and testis.
Rates of New Cancer Cases Fall in 2020 During the COVID-19 Pandemic
Healthcare Disruptions Create Drop in New Cancer Diagnoses
The overall rate of new cancer cases in 2020 was 425.6 per 100,000 people, which is about 8% lower than the 4-year aggregated rate of new cancer cases from 2017 - 2019 and 2021. Rates of new cancer cases were lower across every major site.
Among men, new cancer cases of the larynx and colon and rectum, along with melanoma of the skin, had the largest drops in new diagnoses in 2020 — 10%, 11%, and 12% lower rates, respectively — compared to the 4-year rates. Among women, new cancer cases of the thyroid, stomach, lung and bronchus, colon and rectum, and melanoma of the skin had the largest drops at 13%, 12%, and 10% for each of the remaining three sites.
During 2020, the rates of new cancer cases were highest in January and February and lowest in March, April, and May. April in particular had the lowest overall rate of new cases that year. The rate of new cases returned to expected levels across all sites in 2021.
With the pandemic-related disruptions to the healthcare system, rates of late-stage cancer at diagnosis across all sites increased slightly in 2020 and then decreased slightly in 2021. However, rates of late-stage cervical cancer increased from between 52% and 53.4% during 2017 - 2019 to 57.4% in 2020 and 57.7% in 2021.
Examining Changing Cancer Trends: Incidence and Mortality Falling for Smoking-Related Cancers, Increasing Incidence in Excess Body Weight-Related Cancers
Lung Cancer Mortality Continues to Drop; Progress Slows for Several Cancers Due to Obesity and Other Risk Factors
Declining rates of tobacco use are driving falling rates of new cases and deaths for smoking-related cancers, including lung, bladder, and larynx cancers. Changes in screening recommendations and treatment advances for non-small-cell lung cancer coincide with these falling lung cancer death rates.
Women have rising rates of new cancer cases across more sites than men. However, the increase in stomach cancer cases likely relates to how certain tumors in the stomach — gastrointestinal stromal tumors, or GISTs — are now all classified as malignant. This change happened based on better understanding of these types of rare tumors and does not reflect a change in the underlying cancer burden.
Rates of new cancer cases increased at sites associated with excess body weight, including female breast, uterus, colon and rectum among AYAs, pancreas, kidney, and liver among women.
The reduction in fertility rates, advancing age at first birth, and rises in obesity and alcohol consumption are likely driving rising rates of estrogen receptor-positive breast cancer. About 16% of all breast cancer cases can be linked to alcohol consumption. However, as of 2021, the death rate from breast cancer fell by 42% from its peak in 1989 thanks to treatment and screening advancements.
Rates of new cases and deaths from uterine cancer increased. Risk factors for uterine cancer include excess body weight, physical inactivity, diabetes, and having a first period at an early age. Studies attribute about 53% of all uterine cancer cases in the U.S. to excess body weight and 14% to physical inactivity.
For more detailed information, read the full report here .
.